Scylex Lab
30-Apr-2025
The Science of GLP-1: Metabolism, Medications, and Genetic Insights
The popularity of newer FDA-approved diabetes and weight loss medications has made Glucagon-Like Peptide-1 (GLP-1) a commonly used term. The newer GLP-1 agonist drugs, under brand names like Ozempic, Wegovy, and Zepbound, have emerged as powerful modulators of metabolic health. They’ve proven powerful in improving type 2 diabetes mellitus (T2DM), obesity, and cardiovascular disease (CVD).
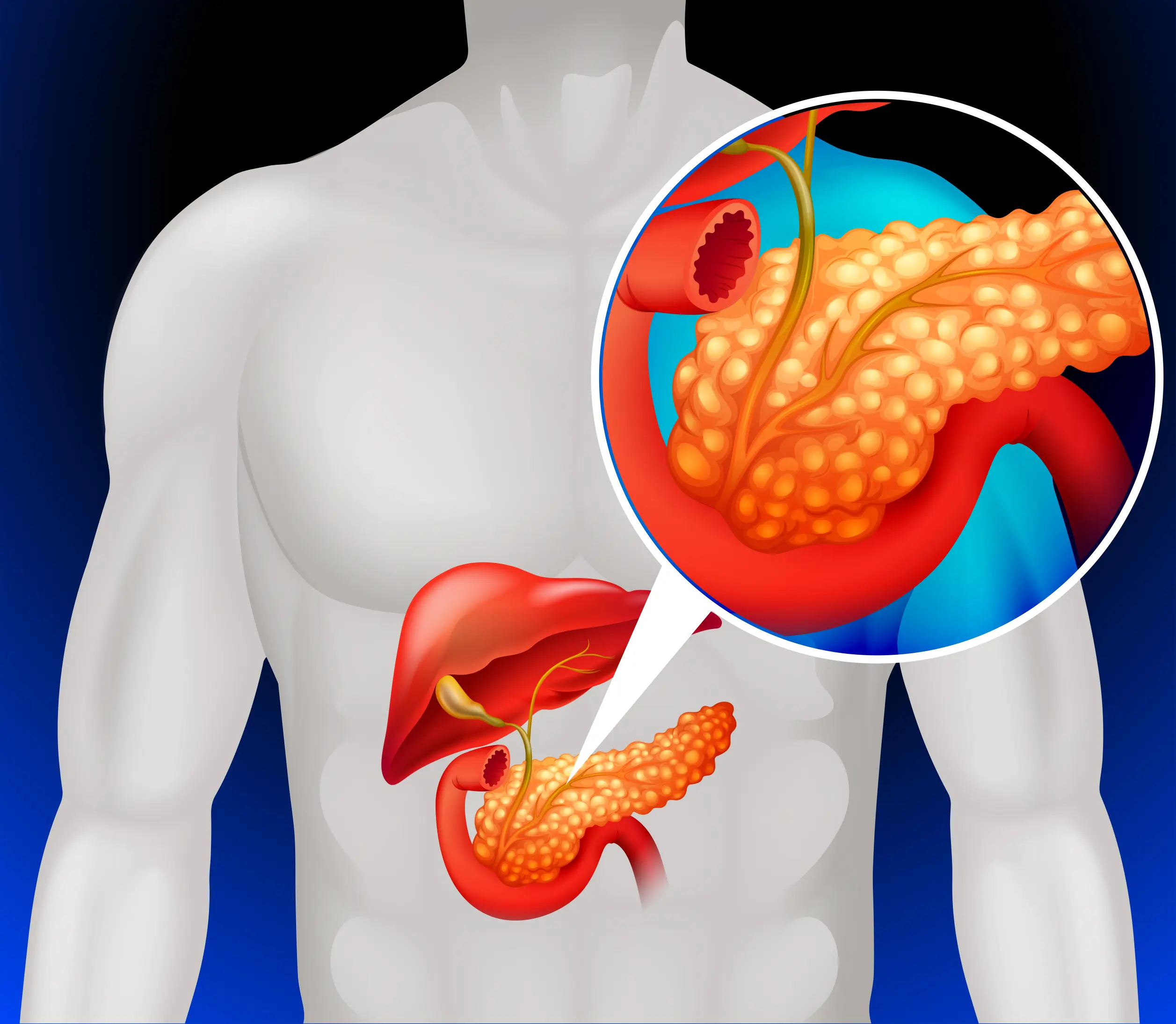
Whether produced endogenously or administered as a medication, GLP-1 enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner and suppresses glucagon release. This works to improve blood sugar management and slow gastric emptying, thereby increasing satiety. These physiological actions place GLP-1 at the crossroads of endocrinology, cardiometabolic and obesity medicine, and emerging fields like nutrigenomics and pharmacogenomics.
GLP-1 and Its Clinical Significance
In response to food intake, GLP-1 is released by intestinal L-cells and acts primarily on the pancreas, where it stimulates insulin secretion from the pancreatic beta cells. In individuals with T2DM, the GLP-1 signaling pathway is often impaired, contributing to elevated blood sugar levels. GLP-1 has also demonstrated cardioprotective effects, including reduced atherosclerotic plaque formation and improved endothelial function. Its ability to reduce appetite and enhance early satiety also makes it an important player in obesity management.
The approval and widespread use of GLP-1 receptor agonists (GLP-1 RAs) such as liraglutide and semaglutide have transformed the treatment landscape for T2DM and obesity. These medications mimic endogenous GLP-1 activity, leading to improved glycemic control, weight loss, and, in some cases, improvement in cardiovascular health.
Genetic Variability in Response to GLP1 RAs
The therapeutic efficacy and tolerability of GLP-1 RAs can be influenced by individual genetic differences, particularly single-nucleotide polymorphisms (SNPs) in the GLP1R gene, which encodes the GLP-1 receptor. These polymorphisms can affect receptor expression, ligand binding, and downstream signaling.
For example, the rs6923761 variant in GLP1R has been associated with altered response to GLP-1 RAs. Carriers of a specific version of this gene may exhibit enhanced insulin secretion and greater weight loss in response to GLP-1 therapy compared to those with other genotypes. Another SNP, rs10305420, has been linked to differential HbA1c response in patients treated with the medication Exenatide for diabetes management. Other SNPs are correlated with an increased risk of adverse gastrointestinal side effects.
Understanding these genetic variations offers a path toward more personalized treatment strategies. By incorporating GLP1R SNP analysis into clinical decision-making, healthcare providers can better predict therapeutic outcomes, optimize medication choice, and minimize adverse effects.
Practical Recommendations for Healthcare Providers
Incorporate genomic testing into comprehensive metabolic assessments to inform personalized nutrition and pharmacologic interventions. This includes screening for GLP1R SNPs in patients being considered for GLP-1 RA therapy. Monitor closely for variable therapeutic outcomes in patients with known GLP1R polymorphisms, adjusting therapy as needed.
Assess beta-cell function using C-peptide measurements or insulin secretion assays to help determine one’s insulin-producing capacity, to help determine the appropriateness of GLP-1 RA initiation. Those with reduced beta-cell functioning may experience a dulled response to these therapies.
Educate patients on the role of GLP-1 in appetite regulation, glycemic control, and cardiovascular protection. Encourage adherence to combining diet and lifestyle changes for optimal therapeutic benefit when using GLP-1 drugs.
Summary
GLP-1 is a central player in regulating glucose, weight management, and cardiovascular health. The integration of GLP-1 receptor agonists into clinical practice has significantly advanced the management of T2DM and obesity. However, genetic variability, particularly in the GLP1R gene, can influence individual response to these therapies. By embracing a personalized approach that includes genomic insights, clinicians can enhance medication efficacy and tolerability, improving patient outcomes in metabolic care.
Scylex offers advanced genomic testing panels that include GLP1R SNP analysis, empowering providers to make more informed, personalized treatment decisions.
Written By:
Vanessa Imus, MS, RDN, owner of Integrated Nutrition for Weight Loss
https://inutritioncenter.com/about/